Breast augmentation: treatment of breast hypotrophy
Contents:
DEFINITION, OBJECTIVES AND PRINCIPLES
Hypoplasia of the breast is determined by the underdeveloped volume of the breast in relation to the morphology of the patient. It may be the result of insufficient development of the gland during puberty or occur a second time with a decrease in the volume of the gland (pregnancy, weight loss, hormonal disorders, etc.). Lack of volume can also be associated with ptosis (a "drooped" chest with gland sagging, skin stretching, and areolas too low).
“This malnutrition is often poorly perceived physically and psychologically by the patient, who experiences it as an attack on her femininity, which leads to a change in self-confidence and sometimes to a deep malaise, which can reach a real complex. This is why the intervention proposes to increase the volume of the breast, which is considered too small, through the implantation of prostheses. »
The intervention can be carried out at any age from 18 years. A minor patient is usually not considered fit for surgery. However, this is possible in cases of severe hypoplasia or in the context of reconstruction such as tubular breasts or breast agenesis. This purely aesthetic purpose cannot be covered by health insurance. Only a few rare cases of true breast agenesis (complete lack of breast development) can sometimes hope for Social Security involvement after prior consent.
Breast implants currently in use consist of a shell and filler. The envelope is always made of silicone elastomer. On the other hand, prostheses differ in their content, that is, in the filler inside the shell. An implant is considered pre-filled if the filler was included at the factory (gel and/or physiological serum). Therefore, the range of different volumes is set by the manufacturer. Saline-inflated implants are filled by the surgeon, who can adjust the volume of the prosthesis to some extent during the procedure.
NEW GENERATION PRE-FILLED SILICONE IMPLANTS
The vast majority of prostheses currently being fitted in France and around the world are pre-filled with silicone gel.
“These implants, which have been in use for over 40 years, have proven to be harmless and highly adaptable to this type of surgery, as they are very close in consistency to normal breasts. They also went through significant changes, especially in the late 1990s, to correct the shortcomings they could be blamed for. Today, all implants available in France meet precise and strict standards: CE marking (European Community) + ANSM (National Agency for the Safety of Medicines and Health Products) approval. »
They consist of a soft silicone gel surrounded by a waterproof, durable and flexible silicone elastomer shell that can be smooth or textured (rough). Significant improvements to the new implants, giving them greater reliability, relate to both shells and the gel itself:
• shells, now with much stronger walls, prevent gel from "bleeding" out (which was the main source of shells) and are much more resistant to wear;
• "Sticky" silicone gels, whose consistency is less liquid, significantly reduce the risk of spread in the event of a sheath rupture.
Along with this increase in reliability, the new generation of silicone implants is also characterized by the wide variety of shapes currently available, allowing them to be individually tailored to each individual case. So, next to the classic round prostheses, “anatomical” implants appeared, profiled in the form of a drop of water, more or less high, wide or protruding. This great variety of shapes, combined with a wide choice of volumes, allows an almost "individual" selection of prostheses to be optimized and adapted to the patient's morphology and personal expectations.
OTHER TYPES OF IMPLANTS
The shells of prostheses are always made of silicone elastomer, the filling is different. To date, only two alternatives to silicone gel are allowed in France: Physiological serum: this is salt water (constituting 70% of the human body). These prostheses may be "pre-filled" (at the factory) or "inflatable" (by the surgeon during surgery). Due to their fluid (rather than gelatinous) content, they have an unnatural consistency, form many more tactile, even visible "folds" and can often be victims of sudden and sometimes early deflation. Hydrogel: This is the latest substance to be approved by Afssaps in 2005. It is an aqueous gel composed primarily of water thickened with a cellulose derivative. This gel, which has a more natural consistency than normal saline, is also absorbed by the body in the event of a membrane rupture. Finally, there are prostheses whose silicone shell is coated with polyurethane, which can help reduce the incidence of shell events.
BEFORE INTERVENTION
Depending on this anatomical context, the preferences and habits of the surgeon, and the wishes expressed by the patient, an operative strategy will be agreed upon. Thus, the location of the scars, the type and size of the implants, as well as their position in relation to the muscle will be predetermined (see below). The preoperative blood test will be carried out as prescribed. The anesthesiologist will attend the consultation no later than 48 hours before the operation. X-ray examination of the breast (mammography, ultrasound) is prescribed. It is strongly recommended to stop smoking at least one month before and one month after the operation (tobacco can delay healing). Do not take medicines containing aspirin for ten days before the operation. You will likely be asked to fast (do not eat or drink anything) for six hours before the procedure.
TYPE OF ANESTHESIA AND METHODS OF HOSPITALIZATION
Type of anesthesia: Most often this is a classic general anesthesia during which you are completely asleep. In rare cases, however, "vigilant" anesthesia (local anesthesia enhanced with intravenous tranquilizers) may be used (in agreement with the surgeon and anesthesiologist). Modes of hospitalization: the intervention usually requires a one-day hospitalization. Entry is then made in the morning (or sometimes the day before) and exit is allowed the next day. However, in some cases, the intervention can be performed "on an outpatient basis", that is, with departure on the same day after several hours of observation.
INTERVENTION
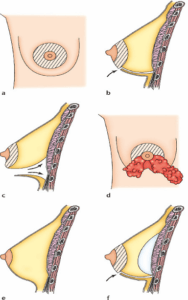
Each surgeon uses his own technique and adapts it to each individual case in order to achieve the best results. However, we can keep the general basic principles: Skin incisions: there are several possible "approaches":
• areolar airways with an incision in the lower segment of the areola circumference or a horizontal hole around the nipple from below (1 and 2);
• axillary, with an incision under the arm, in the armpit (3);
• submammary path, with an incision in the groove located under the breast (4). The path of these incisions obviously corresponds to the location of future scars, which will therefore be hidden at the junctions or in natural folds.
Placement of prostheses
Passing through the incisions, the implants can then be inserted into the created pockets. Two positions are possible:
• premuscular, in which the prostheses are located directly behind the gland, in front of the pectoral muscles;
• retromuscular, in which the prostheses are located deeper, behind the pectoral muscles.
The choice between these two sites, with their respective advantages and disadvantages, should be discussed with your surgeon. Complementary Actions In the case of combined (breast prolapse, low areolas) we have seen that it may be desirable to reduce the skin of the breast in order to make it rise (“mastopexy”). This skin resection will result in larger scars (around the areola ± vertically). Drains and dressings Depending on the habits of the surgeon, a small drain may be placed. This device is designed to evacuate blood that may accumulate around prostheses. At the end of the operation, a “modeling” bandage is applied with an elastic bandage. Depending on the surgeon, the approach and the possible need for accompanying additional procedures, the procedure can last from one hour to two and a half hours.
AFTER THE INTERVENTION: OPERATIONAL OBSERVATION
The postoperative course can sometimes be painful during the first few days, especially with large volume implants and especially when placed behind the muscles. Pain medication adapted to the intensity of the pain will be prescribed for several days. At best, the patient will feel a strong sense of tension. Edema (swelling), ecchymosis (bruising), and difficulty lifting the arms are common in the early stages. The first bandage is removed after a few days. Then it is replaced with a lighter bandage. Then for a few weeks, wearing a bra day and night can be recommended. In most cases, the sutures are internal and absorbable. Otherwise, they will be deleted after a few days. Recovery should be envisaged with a break in activities for five to ten days. It is advisable to wait one to two months to resume sports activities.
RESULT
To evaluate the final result, a period of two to three months is required. This is the time required for the breast to regain flexibility and stabilize the prostheses.
“The operation allowed to improve the volume and shape of the chest. Scars are usually very inconspicuous. The increase in breast volume affects the overall silhouette, providing greater freedom in clothing. In addition to these physical improvements, the restoration of full and whole femininity often has a very beneficial effect on a psychological level. »
The goal of this operation is improvement, not perfection. If your wishes are realistic, the result should please you very much. Stability of the result Regardless of the age of the prostheses (see below) and except for the occurrence of significant weight variation, breast volume will remain stable in the long term. However, with regard to the shape and "holding" of the breast, the "enlarged" breast will be subjected, like a natural breast, to the effects of gravity and aging at different rates depending on the age and quality of skin support, as well as the volume of the breast. implants.
DISADVANTAGES OF THE RESULT
Sometimes some defects may occur:
• residual volume asymmetry, incompletely corrected despite implants of different sizes; • too much rigidity with insufficient flexibility and mobility (especially with large implants);
• somewhat artificial appearance, especially in very thin patients, with excessive visibility of the edges of the prosthesis, especially in the upper segment;
• Sensitivity to the touch of implants is always possible, especially with a small thickness of the tissue cover (skin + fat + iron) covering the prosthesis (especially with large implants).
• there may be an increase in breast ptosis, especially when using large implants. In case of dissatisfaction, some of these shortcomings can be corrected by surgical correction after a few months.
OTHER QUESTIONS
Pregnancy/Breastfeeding
After the installation of breast prostheses, pregnancy is possible without any danger to either the patient or the child, but it is recommended to wait at least six months after the intervention. As for breastfeeding, it is also not dangerous and in most cases remains possible.
Autoimmune diseases
The very numerous international scientific papers carried out on a large scale on this topic have unanimously demonstrated that the risk of this type of rare disease in patients with implants (especially silicone ones) is no higher than in the general female population.
Dentures and cancer
– Until recently, the state of science suggested that the implantation of breast prostheses, including silicone ones, does not increase the risk of developing breast cancer. This is indeed still the case for the most common types of breast cancer (adenocarcinomas, which do not increase in incidence with a breast prosthesis.
However, in the context of cancer screening after implantation, clinical examination and palpation may be impaired, especially in the case of a periprosthetic sheath or siliconoma. Similarly, the presence of implants can interfere with the performance and interpretation of screening mammograms, which should be done regularly. Therefore, you should always indicate that you have breast implants. Thus, depending on the case, certain specialized radiological techniques (specific projections, digitized images, ultrasound, MRI, etc.) can be used. In addition, in case of diagnostic doubt regarding breast cancer, one should be aware that the presence of prostheses may require a more invasive examination to obtain diagnostic certainty.
– Anaplastic large cell lymphoma (ALCL) associated with breast implants (ALCL-AIM) is an exceptional clinical form that has recently been individualized. This entity should only be sought in the case of proven clinical signs (recurrent periprosthetic effusion, breast redness, breast enlargement, palpable mass). Then it is necessary to conduct an accurate senological assessment to clarify the nature of the lesion. In almost 90% of cases, this condition has a very good prognosis and is usually cured by appropriate surgical treatment, combining the removal of the prosthesis and the periprosthetic capsule (total and total capsulectomy). In about 10% of cases, the pathology is more serious and requires treatment with chemotherapy and/or radiation therapy in a team that specializes in the treatment of lymphomas.
Service life of implants
Even if we can see that some patients keep their implants for several decades without major changes, the placement of breast prostheses should not be considered as something definitive "for life". Thus, a patient with implants may expect to have to replace their prostheses one day in order to maintain a positive effect. Implants, whatever they may be, have an indefinite lifespan that cannot be accurately estimated because it depends on the phenomenon of wear at a variable rate. Therefore, the service life of implants cannot be guaranteed. However, it should be noted that new generation implants have made significant progress in terms of strength and reliability. From the tenth year, it will be necessary to raise the question of changing prostheses when a modification of the consistency appears.
watching
It is very important to have the examinations ordered by your surgeon for several weeks and then months after implantation. Subsequently, the presence of implants does not exempt from routine medical supervision (gynecological supervision and breast cancer screening), even if it does not require additional examinations associated with this supervision. However, it is important to let the various doctors know that you have breast prostheses. A consultation with a plastic surgeon about implants is recommended every two to three years, but apart from this follow-up, it is first of all important to come and consult as soon as a modification of one or both breasts is detected. or after a severe injury.
POSSIBLE COMPLICATIONS
Breast augmentation with prostheses, although performed for purely aesthetic reasons, is nevertheless a real surgical procedure that comes with risks associated with any medical procedure, no matter how minimal they may be. A distinction must be made between complications associated with anesthesia and complications associated with surgery: With regard to anesthesia, during the obligatory preoperative consultation, the anesthesiologist himself informs the patient about the anesthetic risks. You should know that anesthesia, whatever it is, causes reactions in the body that are sometimes unpredictable and more or less easily controlled. However, with the assistance of a competent anesthesiologist-resuscitator working in a truly surgical context, the risks became statistically very low. It should indeed be kept in mind that techniques, anesthetics, and monitoring methods have made tremendous progress over the past thirty years, offering optimal safety, especially when the intervention is performed outside the emergency room and in a healthy individual; As for the surgical gesture, by choosing a qualified and competent plastic surgeon trained in this type of intervention, you limit these risks as much as possible, but do not eliminate them completely. In practice, the vast majority of breast augmentation operations carried out within the rules go without problems, the postoperative course is simple, and the patients are completely satisfied with their results. However, sometimes complications can occur during the intervention, some of which are associated with breast surgery, and others are specifically with implants:
Complications inherent in breast surgery
• Effusions, infection-hematoma: The accumulation of blood around the prosthesis is an early complication that can occur in the first hours. If this is important, then it is preferable to return to the operating room to evacuate the blood and stop the bleeding at the site of its origin;
– serous effusion: accumulation of lymphatic fluid around the prosthesis is a fairly common phenomenon, often accompanied by significant edema. This simply results in a temporary increase in breast volume. Disappears spontaneously and gradually;
– infection: rare after this type of surgery. It cannot be resolved with antibiotic therapy alone and then requires surgical revision to drain and remove the implant for several months (the time required to install a new prosthesis without risk). Three other specific forms of infection can also be mentioned:
- late "quiet" infection: this is an infection with few symptoms and no obvious manifestation on examination, which can sometimes occur several years after implantation;
- microabscesses: more often develop at the site of the suture and quickly resolve after removal of the incriminated thread and local treatment;
- Staphylococcal toxic shock: extremely rare cases of this severe generalized infectious syndrome have been reported.
• Cutaneous necrosis Occurs as a result of insufficient tissue oxygenation due to localized insufficient blood supply, which may be contributed to by excessive exertion, hematoma, infection, or heavy smoking in the patient. This is a very rare but dangerous complication, since in extreme cases it can lead to local exposure of the prosthesis, in particular, due to the divergence of the sutures. Revision surgery is often required, sometimes requiring temporary removal of the implant.
• Healing anomalies The healing process involves rather random phenomena, sometimes it happens that in the long term the scars are not as invisible as expected, which then can take on a variety of aspects: dilated, retractile, soldered, hyper- or hypopigmented, hypertrophic (swollen ) or even exclusively keloid.
• Changing the sensitivity. They are frequent in the first months, but most often regress. However, in rare cases, some degree of dysesthesia (reduction or increased sensitivity to touch) may persist, especially in the areola and nipple area. • Galactorrhea/milk effusion Very rare cases of unexplained postoperative hormonal stimulation resulting in milk flow (“galactorrhea”) with occasional fluid around the prosthesis have been reported.
• Pneumothorax Rare, requires special treatment.
Risks associated with implants
• The formation of "folds" or the appearance of "waves"Since the implants are flexible, it is possible that their shell will wrinkle, and these folds can be felt or even visible under the skin in certain positions, giving the impression of waves. This phenomenon is most common in lean patients and can be treated with lipomodelling, which involves applying a thin layer of fat under the skin of the breast to "mask" the implant.
•"Shells
The physiological, normal and permanent reaction of the human body to the presence of a foreign body is to isolate it from surrounding tissues by forming an airtight membrane that surrounds the implant and is called the "periprosthetic capsule". Normally, this shell is thin, flexible and inconspicuous, but it happens that the reaction intensifies and the capsule thickens, becomes fibrous and retracts, squeezing the implant, then called the "shell". Depending on the intensity of the phenomenon, this can lead to: a simple hardening of the breast, sometimes an annoying constriction, even a visible deformity with globulization of the prosthesis, which leads to an extreme degree in a hard, painful, more or less eccentric area. This retractile fibrosis is sometimes secondary to hematoma or infection, but in most cases its occurrence remains unpredictable as a result of random organic reactions.
In recent years, great progress has been made in terms of surgical technique, but above all in the design and construction of implants, resulting in a very significant reduction in the rate and intensity of indentation. If necessary, reoperation can correct such a contracture by cutting the capsule ("capsulotomy").
• Rupture We have seen that implants cannot be considered permanent. Therefore, over time, there may be a loss of tightness of the shell. It can be simple porosity, pinholes, microcracks, or even real holes. In very rare cases, this may be the result of severe trauma or accidental puncture and, more often, the result of progressive wear of the wall due to old age. In all cases, this leads to a possible outcome of the prosthesis filling product, with different consequences depending on the nature of this content:
- with saline or resorbable hydrogel, partial or complete deflation, rapid or rapid deflation is observed;
– with silicone gel (non-absorbable), it remains inside the membrane that isolates the prosthesis. This can then contribute to the appearance of the hull, but it can also remain without consequences and go completely unnoticed. However, in some cases, which have become much rarer (in particular, due to the better “adhesion” of modern gels), one can observe a gradual penetration of the gel into the surrounding tissues. The rupture of the prosthesis most often requires intervention to replace the implants.
• Improper position, misalignment Improper position or secondary misalignment of the implants, which then affects the shape of the breast, can sometimes justify surgical correction.
• Rotation Although rotation of an “anatomical” prosthesis is relatively rare in practice, it is theoretically possible and may affect the esthetic result.
• Deformation of the chest wall. In rare cases, fibrous shell prostheses left in place for long periods of time can "imprint" into the tissues, leaving a deformity of the chest wall that is difficult to correct when removed.
• Late periprosthetic seroma. In very rare cases, a late effusion may form around the prosthesis. Such a late effusion, especially if it is associated with other clinical anomalies of the mammary gland, requires a senological evaluation by a senologist radiologist. The baseline assessment will include ultrasound with effusion puncture. The liquid brought in this way will be the subject of research with the search for lymphoma cells. Digital mammography and/or MRI may be necessary depending on the results of the first fibrous periprosthesis examinations (capsulectomy) allowing biopsy to look for the very rare breast implant-associated anaplastic large cell lymphoma (ALCL-AIM).
Leave a Reply